Cerebral Palsy
What is cerebral palsy?
In Australia there are approximately 34,000 people with cerebral palsy. Worldwide, the incidence of cerebral palsy is 1 in 700 births. There are currently 17 million people in the world who have cerebral palsy.
For most people with cerebral palsy, the cause is unknown. There is no known cure for cerebral palsy.
Cerebral Palsy Physio Treatment: Comprehensive Guide to Improving Quality of Life
Nurturing Hope and Progress for families and people with cerebral palsy
Cerebral palsy is a complex neurological disorder that affects movement, posture, and muscle coordination. Though it presents challenges, remarkable advancements in physiotherapy have significantly improved the lives of those living with cerebral palsy. In this comprehensive guide, we delve into the world of cerebral palsy physio treatment, exploring the role of physiotherapists, various therapeutic approaches, exercises, and activities that can make a difference in the lives of affected individuals.

Understanding Cerebral Palsy
Cerebral Palsy is a non-progressive disorder that primarily affects a person's ability to control their muscles. The condition is caused by damage to the developing brain, typically during pregnancy, childbirth, or shortly after birth. While the exact cause of CP remains uncertain, some known risk factors include premature birth, low birth weight, infections during pregnancy, and maternal health issues.
Types of Cerebral Palsy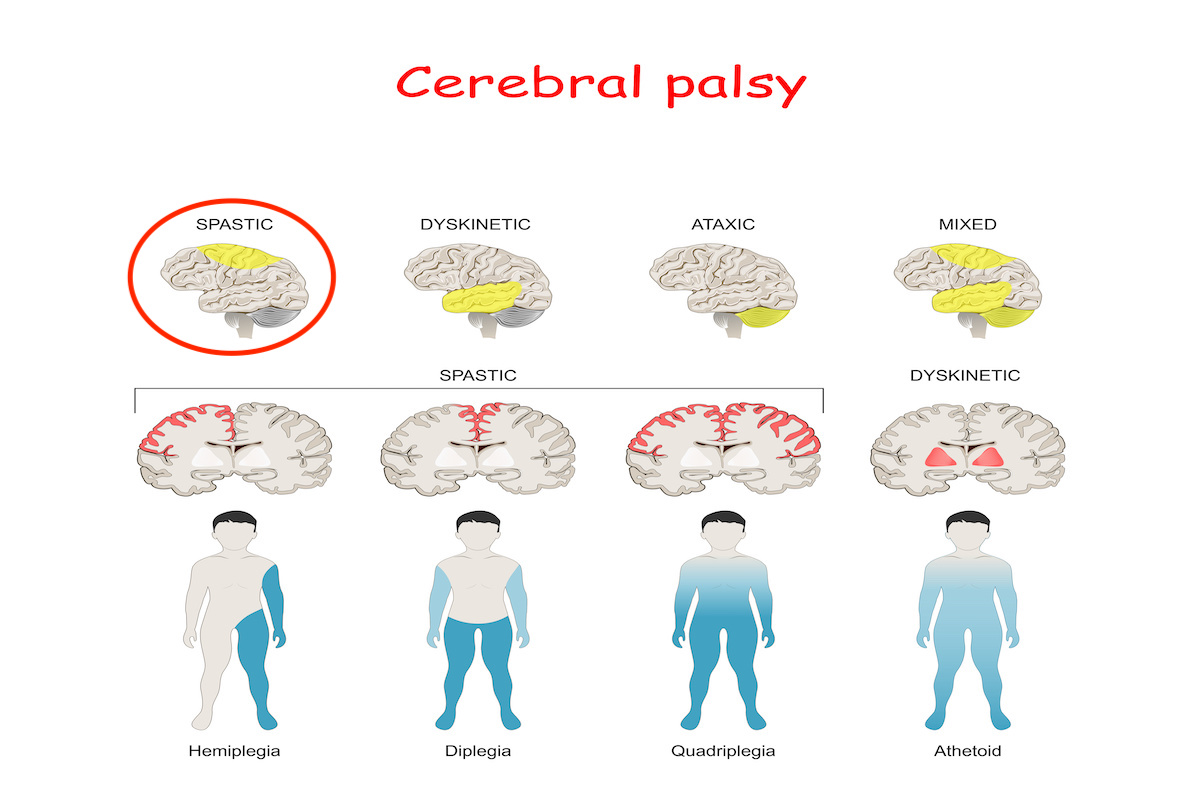
There are several types of Cerebral Palsy, each presenting with different characteristics:
1. Spastic CP
Spastic cerebral palsy is the most common type, characterized by stiff and tight muscles, making movement difficult.
2. Athetoid CP
Individuals with athetoid cerebral palsyexperience involuntary and uncontrolled movements.
3. Ataxic CP
Ataxic cerebral palsyaffects balance and coordination, leading to shaky movements.
4. Mixed CP
Some individuals may have a combination of two or more types, resulting in mixed cerebral palsy.
Causes and Risk Factors
As mentioned earlier, the exact causes of cerebral palsy (CP) are not always known. However, some potential risk factors that can contribute to the development of CP include:
- Infections during pregnancy
- Lack of oxygen to the baby's brain during childbirth
- Premature birth and low birth weight
- Genetic abnormalities
- Brain injuries or infections in early childhood
Diagnosing Cerebral Palsy

Diagnosing a child with CP usually involves a detailed assessment of the child's medical history, developmental milestones, and physical examination. Imaging tests, such as MRI or CT scans, can help identify brain abnormalities or injuries. Early diagnosis by a physiotherapist or physical therapist of a child with cerebral palsy is essential to begin timely intervention and improve outcomes.
Cerebral Palsy Physio Treatment: Understanding the Role of a Physiotherapist
A physiotherapist is a highly skilled professional specializing in helping individuals with cerebral palsy improve their physical abilities and overall quality of life. They assess the specific needs of each patient and create personalized treatment plans to address mobility, strength, and functional limitations. Through a combination of exercises, therapeutic techniques, and adaptive equipment, physiotherapists aim to maximize independence and optimize physical functioning.
Importance of Physiotherapy for individuals with cerebral palsy
Physiotherapy is crucial for the management of Cerebral Palsy as it can:
- Improve muscle tone and flexibility
- Enhance coordination and balance
- Reduce pain and discomfort
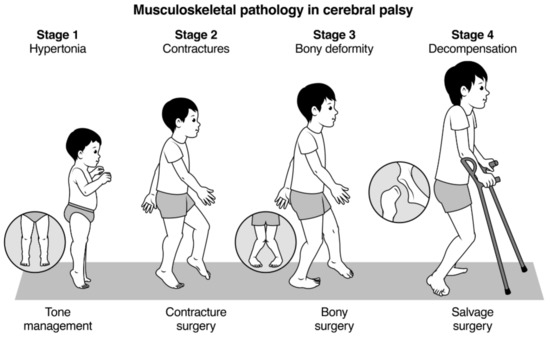
- Prevent complications, such as contractures
- Boost self-esteem and confidence
- Facilitate greater independence in daily life
Components of Cerebral Palsy Physio Treatment
Cerebral Palsy Physio Treatment involves a multi-faceted evidence based approach tailored to the individual's specific needs. Some essential components include:
Therapeutic Exercises
Customized therapeutic exercises target specific muscle groups and help improve strength and flexibility.
Assistive Devices
The use of assistive devices, such as braces or walkers, can provide support and enhance mobility.
Gait Training
Gait training focuses on improving walking patterns, making movements more efficient and stable.
Stretching and Strengthening
Stretching exercises help maintain muscle length, while strengthening exercises build muscle power.
Hydrotherapy
Aquatic therapy (hydrotherapy) in warm water helps reduce muscle tension and supports movement without putting excessive strain on the joints.
Adaptive Recreation
Adaptive recreational activities promote socialization and provide enjoyable opportunities for physical activity.
Speech and Language Therapy
For individuals with speech difficulties, speech therapy aids in developing communication skills.
Occupational Therapy
Occupational therapy focuses on developing skills for daily living and increasing independence.
Nutritional Support
A well-balanced diet with proper nutrients supports overall health and aids in managing weight.
Parental Involvement
Involving parents and caregivers is essential for continued progress and support outside therapy sessions.
What Kind of Physiotherapy therapy is Used for Cerebral Palsy?
Physiotherapy for cerebral palsy encompasses a range of therapeutic approaches tailored to each individual's unique needs. Some common physiotherapy methods include:
1. Neurodevelopmental Treatment (NDT):
NDT is a hands-on therapeutic approach focused on normalizing muscle tone, improving posture, and promoting movement patterns. It encourages the brain to rewire neural pathways, enhancing motor skills and reducing abnormal movements.
2. Constraint-Induced Movement Therapy (CIMT):
CIMT is designed to encourage the use of the affected limbs by restraining the unaffected ones. This therapy promotes functional independence and helps rewire the brain to incorporate the affected limbs in daily activities.
3. Aquatic Therapy:
Aquatic therapy takes advantage of the buoyancy of water to reduce pressure on joints and promote movement in a controlled environment. This therapy can improve muscle strength, flexibility, and cardiovascular fitness.
4. Bobath (Neuro-Developmental Treatment):
The Bobath approach focuses on improving posture and movement patterns, using gentle, hands-on techniques to influence muscle tone and motor control.
5. Functional Electrical Stimulation (FES):
FES involves using electrical currents to stimulate nerves and muscles, helping individuals with cerebral palsy improve muscle strength and coordination.
6. Hippotherapy:
Hippotherapy involves horse riding, which can provide sensory stimulation and improve balance, coordination, and core strength.
The Management and Main Aim of Physiotherapy in CP is to Improve:
The primary goal of physiotherapy in cerebral palsy is to improve the overall functional abilities and quality of life for affected individuals. Physiotherapists work towards achieving the following objectives:
- Enhancing Mobility:
Physiotherapy focuses on improving mobility, gait, and coordination to help individuals move more independently and efficiently.
- Reducing Pain and Discomfort:
Through a combination of therapeutic techniques and exercises, physiotherapy can alleviate pain and discomfort associated with cerebral palsy.
- Increasing Muscle Strength:
Physiotherapists design targeted exercises to strengthen muscles, promoting better control and stability.
- Enhancing Flexibility:
Stretching exercises are an integral part of physiotherapy, promoting flexibility and preventing contractures.
- Improving Balance and Posture:
Correcting postural imbalances and enhancing balance are crucial to minimizing the risk of falls and injuries.
- Promoting Independence in Daily Activities:
Physiotherapy aims to help individuals perform daily tasks independently, boosting their self-esteem and confidence.
Which Therapy is Best for Cerebral Palsy.. Physiotherapy can help
The choice of therapy for cerebral palsy depends on the severity of the condition and individual needs. Each therapy has its strengths, and a comprehensive approach may combine multiple techniques to achieve optimal results. It's essential to consult a qualified physiotherapist who can assess the specific requirements and recommend the most suitable therapy.
How Do You Rehabilitate Cerebral Palsy?
Rehabilitation for cerebral palsy involves a multi-disciplinary approach, with physiotherapy playing a crucial role. The rehabilitation process may include:
- Evaluation and Assessment:
A comprehensive evaluation is conducted to determine the individual's current abilities, limitations, and potential for improvement.
- Goal Setting:
Based on the assessment, specific functional goals are set, focusing on improving mobility, strength, and daily living activities.
- Personalized Treatment Plan:
A personalized treatment plan is created, incorporating various physiotherapy techniques and exercises.
- Regular Therapy Sessions:
Individuals typically undergo regular therapy sessions to work towards their goals and measure progress.
- Home Exercises:
Patients are often prescribed home exercises to complement their therapy sessions and maintain progress.
How Do You Strengthen Cerebral Palsy?
Strengthening exercises are a crucial component of cerebral palsy physio treatment. Some effective strengthening exercises include:
1. Weight Bearing Exercises:
Exercises that involve bearing weight on the arms or legs can strengthen muscles and improve bone density.
2. Resistance Training:
Resistance bands or light weights can be used to increase muscle strength gradually.
3. Core Strengthening:
Targeting the core muscles improves stability and posture, aiding in overall strength and balance.
4. Functional Exercises:
Functional exercises mimic daily activities, enhancing muscle coordination and promoting independence.
What Activities Help Cerebral Palsy?
Engaging in specific activities can significantly benefit individuals with cerebral palsy:
- Swimming:
Swimming provides an excellent full-body workout while reducing pressure on joints, promoting muscle strength, and enhancing cardiovascular fitness.
- Cycling:
Cycling with adapted bikes can improve leg strength, coordination, and overall endurance.
- Yoga:
Yoga enhances flexibility, balance, and relaxation, providing a holistic approach to cerebral palsy physio treatment.
- Dancing:
Dancing can be an enjoyable way to improve motor skills, coordination, and self-expression.
Can Cerebral Palsy Improve with Exercise?
Yes, cerebral palsy can improve with appropriate exercises and therapy. Regular physiotherapy sessions and targeted exercises can help individuals enhance their physical abilities, increase muscle strength, and achieve better functional independence.
Can You Build Muscle with Cerebral Palsy?
Absolutely! With consistent and targeted strength-building exercises, individuals with cerebral palsy can build muscle and improve their overall physical capabilities.
What Can Make Cerebral Palsy Worse?
Several factors can exacerbate cerebral palsy symptoms:
- Lack of Regular Exercise:
A sedentary lifestyle can lead to muscle weakness and reduced mobility.
- Poor Nutrition:
A balanced diet is crucial for maintaining optimal health and supporting the body's natural functions.
- Ignoring Medical Advice:
Regular medical check-ups and adherence to treatment plans are vital for managing cerebral palsy effectively.
What Can People with Cerebral Palsy Not Do?
While individuals with cerebral palsy may face challenges, it is essential to focus on their abilities rather than limitations. Each person's capabilities vary, and with appropriate support and encouragement, they can lead fulfilling lives, engaging in a range of activities.
What is Hard for People with Cerebral Palsy?
The challenges faced by individuals with cerebral palsy may include:
- Mobility Issues:
Difficulty with walking, balance, and coordination may hinder independent movement.
- Speech and Communication Challenges:
Some individuals may have difficulty speaking or communicating effectively.
- Fine Motor Difficulties:
Tasks requiring precise hand and finger movements might be challenging.
- Social and Emotional Factors:
Navigating social situations and building relationships can be complex.
Conclusion: Empowering Lives Through Physiotherapy
Cerebral palsy physio treatment offers hope and progress for individuals living with this condition. Physiotherapists play a vital role in designing personalized treatment plans to improve mobility, strength, and overall well-being. Through a range of therapeutic approaches, exercises, and activities, individuals with cerebral palsy can enhance their quality of life and achieve greater independence. Remember, each individual's journey is unique, and with the right support, people with cerebral palsy can lead fulfilling lives.
FAQs
How Do You Strengthen Cerebral Palsy?
Strengthening exercises are essential for individuals with cerebral palsy. Activities like weight-bearing exercises, resistance training, and core strengthening can significantly improve muscle strength, stability, and overall physical abilities.
Can Cerebral Palsy Improve with Exercise?
Yes, cerebral palsy can improve with regular exercise and physiotherapy. Targeted exercises can enhance muscle strength, coordination, and functional independence, leading to an improved quality of life.
What Can Make Cerebral Palsy Worse?
Factors like a lack of regular exercise, poor nutrition, and ignoring medical advice can exacerbate cerebral palsy symptoms. It's crucial to maintain a healthy lifestyle and follow medical recommendations.
What Can People with Cerebral Palsy Not Do?
While individuals with cerebral palsy may face challenges, focusing on their abilities rather than limitations is essential. Each person's capabilities vary, and with proper support, they can engage in various activities.
What is Hard for People with Cerebral Palsy?
People with cerebral palsy may encounter difficulties related to mobility, speech, fine motor skills, and social interactions. However, with understanding and support, they can overcome these challenges and thrive in life.
Which Therapy is Best for Cerebral Palsy?
The best therapy for cerebral palsy varies based on individual needs and the severity of the condition. Physiotherapists can assess and recommend the most suitable therapy for each patient's specific requirements.
References
-
-
Cerebral Palsy Alliance Australia - Physiotherapy Services: https://cerebralpalsy.org.au/services/physiotherapy/ Cerebral Palsy Alliance Australia is a reputable organization dedicated to supporting individuals with cerebral palsy and their families. Their page on physiotherapy services provides valuable information about the role of physiotherapists, evidence-based approaches, and the impact of physiotherapy on improving the quality of life for individuals with cerebral palsy in Australia.
-
Australian Physiotherapy Association - Cerebral Palsy Treatment: https://australian.physio/inmotion/what-cerebral-palsy-and-how-it-treated The Australian Physiotherapy Association (APA) is a leading professional body representing physiotherapists in Australia. Their article on cerebral palsy treatment offers expert insights into the physiotherapy methods used to address cerebral palsy in the country, giving the content added credibility.
-
Better Rehabilitation - Cerebral Palsy Physiotherapy: https://betterrehab.com.au/services/cerebral-palsy-physiotherapy/ Better Rehabilitation is a specialized provider of physiotherapy services for individuals with cerebral palsy in Australia. Their page on cerebral palsy physiotherapy outlines specific approaches, techniques, and programs designed to enhance the functional abilities and overall well-being of affected individuals.
-
Royal Children's Hospital Melbourne - Physiotherapy for Cerebral Palsy: https://www.rch.org.au/physio/clinical_guidelines/Physiotherapy_for_children_with_Cerebral_Palsy/ The Royal Children's Hospital Melbourne is a renowned medical institution providing comprehensive care for children with cerebral palsy. Their page on physiotherapy for cerebral palsy offers evidence-based guidelines and protocols used in the management of the condition, making it a valuable resource for readers seeking expert information.
-
Scope - Physiotherapy Services for Cerebral Palsy: https://www.scopeaust.org.au/services/therapy-services/physiotherapy/ Scope is a disability services provider in Australia with expertise in supporting individuals with cerebral palsy. Their page on physiotherapy services for cerebral palsy outlines the diverse range of therapeutic interventions available, highlighting the importance of tailored approaches for each individual.
- National Institutes of Health (NIH) - Cerebral Palsy Information Page URL: https://www.ninds.nih.gov/Disorders/All-Disorders/Cerebral-Palsy-Information-Page
Why: NIH is a reputable government institution known for its high-quality, evidence-based information on various health conditions, including cerebral palsy. The information provided on their page can further support and validate the content of your comprehensive guide. -
American Physical Therapy Association (APTA) - Cerebral Palsy Resource Center URL: https://www.apta.org/cerebral-palsy
Why: APTA is a professional organization for physical therapists in the United States. Their resource center on cerebral palsy can provide insights into the role of physiotherapists and evidence-based approaches used in the treatment of cerebral palsy. This link can enhance the credibility of your content.
-
Mayo Clinic - Cerebral Palsy Overview URL: https://www.mayoclinic.org/diseases-conditions/cerebral-palsy/symptoms-causes/syc-20353999
Why: Mayo Clinic is a renowned medical institution known for its expertise and reliable healthcare information. Their overview on cerebral palsy can offer readers a deeper understanding of the condition and its various aspects, supporting the information in your guide.
-
World Confederation for Physical Therapy (WCPT) - Cerebral Palsy Management URL: https://www.wcpt.org/sites/wcpt.org/files/files/Guideline_Cerebral_Palsy_0.pdf
Why: WCPT is a global organization representing physical therapists worldwide. Their guideline on cerebral palsy management is based on the latest research and evidence, making it a valuable resource to reinforce the credibility of your content.
-
Centers for Disease Control and Prevention (CDC) - Cerebral Palsy Information URL: https://www.cdc.gov/ncbddd/cp/index.html
Why: The CDC is a reputable source for public health information. Their page on cerebral palsy provides comprehensive information on the condition, including risk factors, diagnosis, and management. Linking to this page can enhance the reliability of your content.
-
United Cerebral Palsy (UCP): https://ucp.org/ United Cerebral Palsy is a non-profit organization dedicated to enhancing the quality of life for individuals with cerebral palsy and other developmental disabilities. Their website offers support, resources, and information about cerebral palsy, making it a trustworthy and valuable source for readers seeking additional assistance and community connections.
-
More About Cerebral Palsy
Types of cerebral palsy
QUADRIPLEGIA (A FORM OF BILATERAL CEREBRAL PALSY)
DIPLEGIA (A FORM OF BILATERAL CEREBRAL PALSY)
HEMIPLEGIA (A FORM OF UNILATERAL CEREBRAL PALSY)
OTHER CLASSIFICATIONS
- Gross motor skills – Gross Motor Function Classification System (GMFCS)
- Fine motor skills – Manual Ability Classification System (MACS)
- Communication – Communication Function Classification System (CFCS)
SPASTIC
- The most common form of cerebral palsy
- Muscles feel stiff and tight
DYSKINETIC
- Characterised by involuntary movements (i.e. out of a person’s control)
ATAXIC
- Characterised by shaky movements
- Affects balance and sense of positioning in space
MIXED TYPE
What causes cerebral palsy?
There is no single cause of cerebral palsy. For most babies born with cerebral palsy, the cause remains unknown.Researchers now know that only a very small percentage of cases of cerebral palsy are due to complications at birth (e.g. asphyxia or lack of oxygen). Today, it is accepted that cerebral palsy usually arises from a series of causal pathways, i.e. a sequence of events that when combined can cause or accelerate injury to the developing brain.
In 13 out of 14 cases of cerebral palsy in Australia, the brain injury leading to cerebral palsy occurs either in the uterus (while the mother is pregnant) or before 1 month of age.
Stroke is the most common cause in babies who acquire cerebral palsy after 1 month of age. The stroke may occur spontaneously or arise from surgical or heart complications.
Key facts about cerebral palsy
- Every 15 hours, an Australian child is born with cerebral palsy.
- It is the most common physical disability in childhood.
- Cerebral palsy is an umbrella term for a group of disorders. It is a condition that is permanent, but not unchanging.
- Cerebral palsy is a life-long physical disability due to damage of the developing brain.
- In most cases, brain injury leading to cerebral palsy occurs during pregnancy.
- Cerebral palsy, except in its mildest forms, can be evident in the first 12-18 months.
- Motor disability can range from minimal to profound, depending on the individual.
- It can range from weakness in one hand, to an almost complete lack of voluntary movement. People with significant physical disability may require 24 hour a day care.
- People with cerebral palsy are likely to also have other impairments in addition to their motor disability.
- Spastic hemiplegia, where one half of the body has difficulty with voluntary movement, is the most common presentation of cerebral palsy. Approximately 40% of people with cerebral palsy have hemiplegia.
- There is no known cure.
How does cerebral palsy affect people?
The parts of the body affected by cerebral palsy, the level of severity and combination of symptoms can differ for each person. For example, one person may have a weakness in one hand and find tasks like writing or tying shoelaces challenging. Another person may have little or no control over their movements or speech and require 24 hour assistance.
People with cerebral palsy may experience uncontrolled or unpredictable movements, muscles can be stiff, weak or tight and in some cases people have shaky movements or tremors. People with severe cerebral palsy may also have difficulties with swallowing, breathing, head and neck control, bladder and bowel control, eating and have dental and digestive problems.
1 in 3 children with cerebral palsy will be unable to walk. At greatest risk are those who have spastic quadriplegia, intellectual disability, epilepsy, vision impairment and an inability to sit independently at 2 years of age.
See:
- Ankle Foot Orthoses
- Conductive education
- Constraint-induced movement therapy for the leg (CIMT-Leg)
- Early motor intervention
- Hydrotherapy for adolescents and adults
- Massage for pain and movement
- Powered mobility
- Treadmill training for people with cerebral palsy
Communication issues
Cerebral palsy can affect a person’s ability to finely coordinate the muscles around the mouth and tongue that are needed for speech. The coordinated breathing that is needed to support speech can also be affected, e.g. some people may sound ‘breathy’ when they speak. Some people with cerebral palsy may not be able to produce any sounds, others may be able to produce sounds but have difficulty controlling their movement enough to produce speech that is clear and understood by others. 1 in 4 people with cerebral palsy cannot talk.
See:
- Communication Partner Training
- Conductive education
- Eye-gaze technology
- Speech generating devices
- Speech therapy for children with dysarthria
Pain
3 in 4 people with cerebral palsy experience pain. Pain is often a result of the impairments that are associated with cerebral palsy, e.g. contractures, abnormal postures, dystonia, skin breakdown, hip subluxation, Gastro-oesophageal reflux and scoliosis. This pain can affect a person’s behavior, their ability to do things for themselves, to sleep and their social relationships. People might avoid day-to-day tasks that are important for independence, such as attending school and social events. Pain can be relieved, so it is best to be guided by your medical practitioner.
See:
- Botulinum Toxin-A injections for supporting pain and comfort
- Cognitive-behaviour therapy for pain
- Gastrostomy feeding
- Hydrotherapy for adolescents and adults
- Massage for pain and movement
- Sleep positioning systems
Eating and drinking issues
Cerebral palsy can affect the muscles that open and close the mouth and move the lips and the tongue. Some people with cerebral palsy may have difficulties in chewing and swallowing food and drink – a condition known as dysphagia. Because cerebral palsy often impacts fine motor skills, many people are unable to easily use cutlery, hold a cup, or transfer food from a plate to their mouth using their hands. Others may suffer from gastroesophageal reflux – where acid from the stomach rises into the esophagus – which makes eating uncomfortable or painful. This can sometimes be controlled by medication.1 in 15 people with cerebral palsy are unable to take food through their mouth and need to be fed through a feeding tube.
See:
Saliva control
Because cerebral palsy can affect the muscles around the mouth, 1 in 5 children with cerebral palsy have saliva loss (also known as dribbling, drooling or sialorrhoea). The saliva loss may be more noticeable when they are concentrating on doing other tasks.
Intellectual disability
1 in 2 people with cerebral palsy have an intellectual disability. 1 in 5 people have a moderate to severe intellectual disability. Generally, the greater the level of a person’s physical impairment, the more likely it is that they will have an intellectual disability. However, there are people who have a profound level of physical impairment, who do not have an intellectual disability. Conversely, there can be others with a mild physical impairment who have an intellectual disability.
Learning difficulties
Children with cerebral palsy may experience specific learning difficulties. These may include a short attention span, motor planning difficulties (organisation and sequencing of movement), perceptual difficulties and language difficulties. These can impact on literacy, numeracy and other classroom skills and activities. Learning may also be affected by difficulties in fine motor and gross motor coordination and communication. Students with cerebral palsy need to put more effort into concentrating on their movements and sequence of actions than others, so they may tire more easily.
Hearing impairment
1 in 20 people with cerebral palsy also have some level of hearing impairment. 1 in 25 children with cerebral palsy are deaf.
Vision impairment
Vision impairment is not uncommon in people with cerebral palsy. Children with the more severe forms of cerebral palsy are more likely than others to experience myopia, absence of binocular fusion, dyskinetic strabismus (also known as ‘turned eye’ or ‘squint’), severe gaze dysfunction, and optic neuropathy or cerebral visual impairment. 1 in 10 children with cerebral palsy are blind.
Behavior and emotional wellbeing
One in 4 children with cerebral palsy have behaviour problems. At greatest risk are those with an intellectual disability, epilepsy, severe pain or a milder level of physical disability. Problem behaviors include dependency, being headstrong, hyperactive, anxious, or prone to conflict with their peer group, or exhibiting antisocial behaviours. Children with cerebral palsy may also have emotional problems such as difficulties with their peer group and strong emotional responses to new challenges. Teenagers and adults with cerebral palsy may be more prone to depression and anxiety disorders.
See:
- Cognitive behaviour therapy for anxiety
- Counselling at the Time of Diagnosis
- Solution focused brief therapy
- Stepping Stones Triple P parenting program
Epilepsy
1 in 4 children with cerebral palsy have epilepsy. When children have cerebral palsy and an intellectual disability, the incidence of epilepsy is higher – 48%. Seizures can affect speech, intellectual and physical functioning. Medication is the most effective intervention for epilepsy and the child’s doctor or therapist may also recommend modifications to the student’s school supports and equipment. Some medications have side effects which cause drowsiness or irritability. Both epilepsy and the related medication can affect a person’s behavior and attention span.
Sleep issues
1 in 5 children with cerebral palsy have a sleep disorder. There are a range of contributing factors, including the muscle spasms associated with cerebral palsy, other forms of musculo-skeletal pain, and decreased ability to change body position during the night. Epilepsy is also known to disturb sleep and is likely to predispose to sleep disorders. Blindness or severe visual impairment can affect the timing and maintenance of sleep through their effect on melatonin secretion and the lack of light perception.
See:
Spinal and hip abnormalities
Abnormalities of the spine and hips are associated with cerebral palsy and can make sitting, standing and walking difficult, and cause chronic pain. 1 in 3 children with cerebral palsy have hip displacement. Children and adults who have a severe physical disability or those whose body is affected on both sides are at greater risk of hip problems. This means that people who use wheelchairs most of the time are more at risk of hip problems than those who walk with assistive devices or independently.
Bladder and bowel control
Continence and constipation are issues for many people with cerebral palsy. 1 in 4 children with cerebral palsy have bladder control problems. Children with intellectual disability and/or a severe form of cerebral palsy are most at risk. Lack of mobility and difficulty eating can predispose people with cerebral palsy to constipation.
Treatment for cerebral palsy
Children with cerebral palsy may be supported by a team of professionals including health professionals and community-based support services who work together to help the child and family reach their goals.
Through their late teens and early 20s, many young people take increasing responsibility for their own health and wellbeing. Their team may include health professionals and mainstream community providers such as fitness trainers.
Medication
Medical specialists may prescribe medications that assist movement issues. Some medications are taken orally (e.g. diazepam) and others are injected or delivered through surgically implanted pumps (e.g. Baclofen). Many children with cerebral palsy benefit from Botulinum toxin type A injections into muscles affected by spasticity. This intervention is used from about two years of age and is most effective when used in conjunction with therapy.
See:
- Botulinum Toxin-A injections for supporting pain and comfort
- Occupational therapy following botulinum toxin-A injections
Surgical procedures
Selective Dorsal Rhizotomy (SDR) is a neurosurgical procedure that is used in a small percentage of children with cerebral palsy to permanently reduce spasticity in their legs.
Physiotherapy and occupational therapy
Physiotherapists and occupational therapists focus on encouraging a person’s day-to-day movement skills such as sitting, walking, playing, dressing and toileting. They will use a range of specialist interventions such as movement training and equipment, e.g. walking frames, wheelchairs, supportive seating, footwear and orthotics.
See:
- Ankle Foot Orthoses
- Bimanual upper limb therapy
- Conductive education
- Constraint-induced movement therapy for the leg (CIMT-Leg)
- Goal directed training
- Home programs
- Hydrotherapy for adolescents and adults
- Massage for pain and movement
- Powered mobility
- Treadmill training for people with cerebral palsy
Physiotherapists and occupational therapists may also focus on preventing impairments that might affect movement. They use casts, orthotics and muscle strengthening exercises.
See:
Support for people with cerebral palsy
- Your local general practitioner (GP)
- National Disability Insurance Scheme (NDIS): The NDIS is a way of providing funding to individuals with a disability. The goal of the NDIS is to provide you with the resources you need now, so you can build your capacity and independence for the future.
- Services and support through organisations such as CPL - Choice, Passion, Life or FNQ Cerebral Palsy Support Group Inc.
- Physio Labs - Give us a call on 07 5610 1933 to see how we can support you
References
- https://cerebralpalsy.org.au/our-research/about-cerebral-palsy/what-is-cerebral-palsy/
- https://cerebralpalsy.org.au/our-research/about-cerebral-palsy/what-is-cerebral-palsy/types-of-cerebral-palsy/
- https://cerebralpalsy.org.au/our-research/about-cerebral-palsy/what-is-cerebral-palsy/causes/
- https://cerebralpalsy.org.au/our-research/about-cerebral-palsy/what-is-cerebral-palsy/facts-about-cerebral-palsy/
- https://cerebralpalsy.org.au/our-research/about-cerebral-palsy/what-is-cerebral-palsy/how-cerebral-palsy-affects-people/
- https://cerebralpalsy.org.au/our-research/about-cerebral-palsy/what-is-cerebral-palsy/interventions/